Personlig internetbaseret behandling af angst og depression hos patienter med iskæmisk hjertesygdom.
Projektets formål
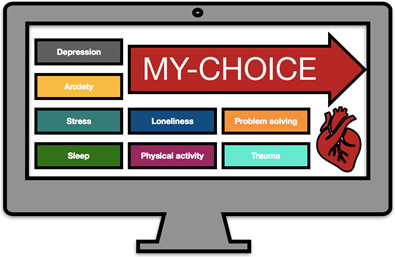
Det overordnede formål med MY-CHOICE projektet er at udvikle og evaluere en personlig, terapeutassisteret eHealth-behandling for depression og angst hos patienter med iskæmisk hjertesygdom, der deltager i hjerterehabilitering. Interventionen er patientcentreret og holistisk, da den ikke kun retter sig mod depression og angst, men også de mest almindelige udfordringer, som patienter står overfor, når de diagnosticeres med iskæmisk hjertesygdom, inklusive træthed, søvnproblemer, bekymringer for fremtiden, eksistentiel krise, og vanskeligheder med at leve efterleve anbefalingerne for sund livsstil.
Interventionen vil delvist være baseret på principperne for kognitiv adfærdsterapi, men vil også inkludere aspekter fra Acceptance and Commitment Therapy og Compassion Focused Therapy. Dog er interventionen fleksibelt målrettet mod den enkelte patients behov og præferencer og er også designet til at inkludere og fastholde socialt udsatte patienter og patienter i risiko for at falde fra. Ud over behandlingsmoduler rettet mod depression og angst har patienter mulighed for at vælge behandlingsmoduler om emner, de ønsker at arbejde med i dialog med deres terapeut, herunder eksistentielle vanskeligheder, ensomhed osv.
Projektet har 2 faser:
Fase 1: Patientmedforskere med IHD og tidligere eller nuværende depression og/eller angst vil samarbejde med kliniske psykologer om at udvikle eHealth-modulerne i MY-CHOICE baseret på præmissen om personlig medicin.
Fase 2: En gennemførlighedundersøgelse af interventionen med 30 patienter.
Baggrund
Iskæmisk hjertesygdom (IHD) er en kronisk sygdom, kendetegnet ved nedsat blodtilførsel til hjertet, som kan føre til akut myokardieinfarkt, hjertesvigt, hjertestop og for tidlig død. Antallet af patienter med IHD er steget eksponentielt på grund af bedre behandlingsmuligheder og en aldrende befolkning, med 21.000 nye patienter diagnosticeret i Danmark hvert år. For at mindske påvirkningen af IHD henvises patienter til hjerterehabilitering, en tværfaglig og mangesidet indsats primært fokuseret på fysisk træning, patientuddannelse og risikofaktorstyring. Men frafaldsraterne er høje med op til 50%, hvilket kræver mere opmærksomhed på hindringer for deltagelse og vedholdenhed i hjerterehabilitering. Studier har vist, at især patienter, der er psykologisk og socialt sårbare, er i risiko for frafald. Så mange som en ud af fem patienter (20%) med IHD udvikler depression og angst, der kræver behandling. Formålet med dette projekt er derfor at optimere rehabilitering i en sådan grad, at flere sårbare patienter deltager i rehabilitering, mens de også modtager behandling for depression og angst.
Forventede resultater
Vi ønsker at give patienterne en mere aktiv rolle som fortalere for deres egen sundhed i behandlingsprocessen, samtidig med at behandlingsanbefalinger kan skræddersys til den enkelte patients behov og præferencer. Vi forventer, at dette vil forbedre patientens empowerment, adherence, behandlingstilfredshed og livskvalitet, og muligvis hjælpe med at forhindre indlæggelser og generelt sætte patienter i stand til at leve et bedre liv med deres sygdom.
Projektteam
Professor Susanne S. Pedersen (PI), psykolog, Institut for Psykologi, Syddansk Universitet og Hjertemedicinsk afdeling, Odense Universitetshospital;
Robert Ahm, psykolog, Institut for Psykologi, Syddansk Universitet;
Søren Jensen Skovbakke, fysioterapeut, Institut for Psykologi, Syddansk Universitet;
Ole Skov, statistiker, Institut for Psykologi, Syddansk Universitet;
Christina Antoinetta Vasilescu, studentermedhjælper, Institut for Psykologi, Syddansk Universitet;
Lotte Helmark, hjertesygeplejerske, kardiologisk afdeling, Sjællands Universitetshospital og Institut for Psykologi, Syddansk Universitet;
Overlæge Helle Lynge Kanstrup, kardiolog, Hjertemedicinsk afdeling, Aarhus Universitetshospital;
Professor Lisbeth Frostholm, psykolog, Klinisk Institut, Aarhus Universitetshospital.
Projektet er støttet med 2 millioner af Karen Elise Jensen Fonden.