Promising Results in Cancer Treatment with Immunotherapy and Danish Technology
A combination of immunotherapy and a newly developed Danish technology is demonstrating promising outcomes for patients with particularly severe breast cancer. This treatment also holds promise for other types of cancer.
Over the past two decades, immunotherapy – utilizing the body's own immune system to combat illness – has emerged as a groundbreaking treatment for various types of cancer. The body's own T-cells possess a remarkable capacity to identify and fight a wide range of cancers. Regrettably, cancer cells frequently develop the ability to weaken the activity of T-cells.
- We already have several drugs that inhibit the weakening of T-cells, but even the most effective drugs vary greatly in effect depending on the type of cancer being treated, explains Odd Gammelgaard, one of the researchers behind the newly published study.
A limiting factor in the use of these drugs is the requirement for patients to have sufficient numbers of so-called reactive T-cells that can distinguish between healthy and diseased cells, which is often not the case. To address this, technologies have been developed that enable the selection and cultivation of T-cells in the laboratory.
Mød forskeren
Odd Gammelgaard is post. doc at the Cancer and Inflammation Research Unit with the Department of Molecular Medicine at SDU.
Cultivated from the Patients' Blood
The Danish biotech company CytoVac has developed a new technology where they draw the patients’ own blood and then isolate and mature T-cells in a laboratory setting. These lab-cultivated T-cells are subsequently reintroduced into the patients.
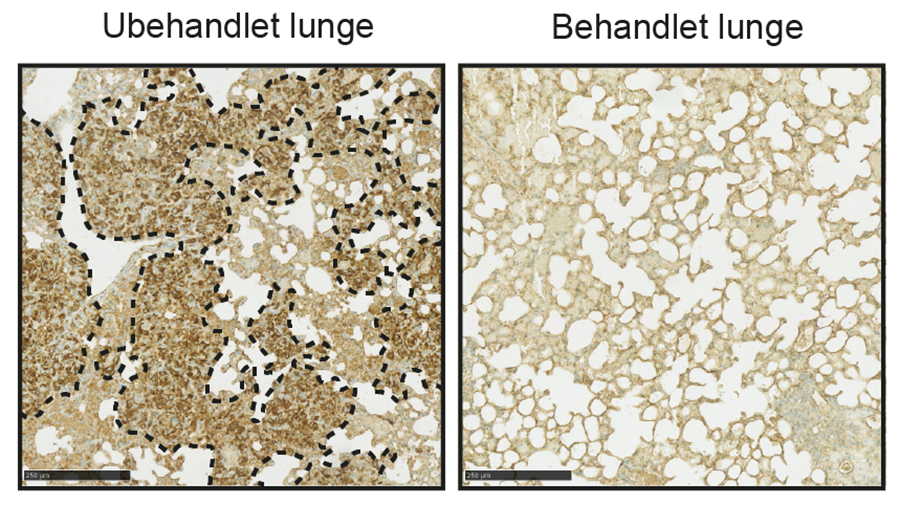
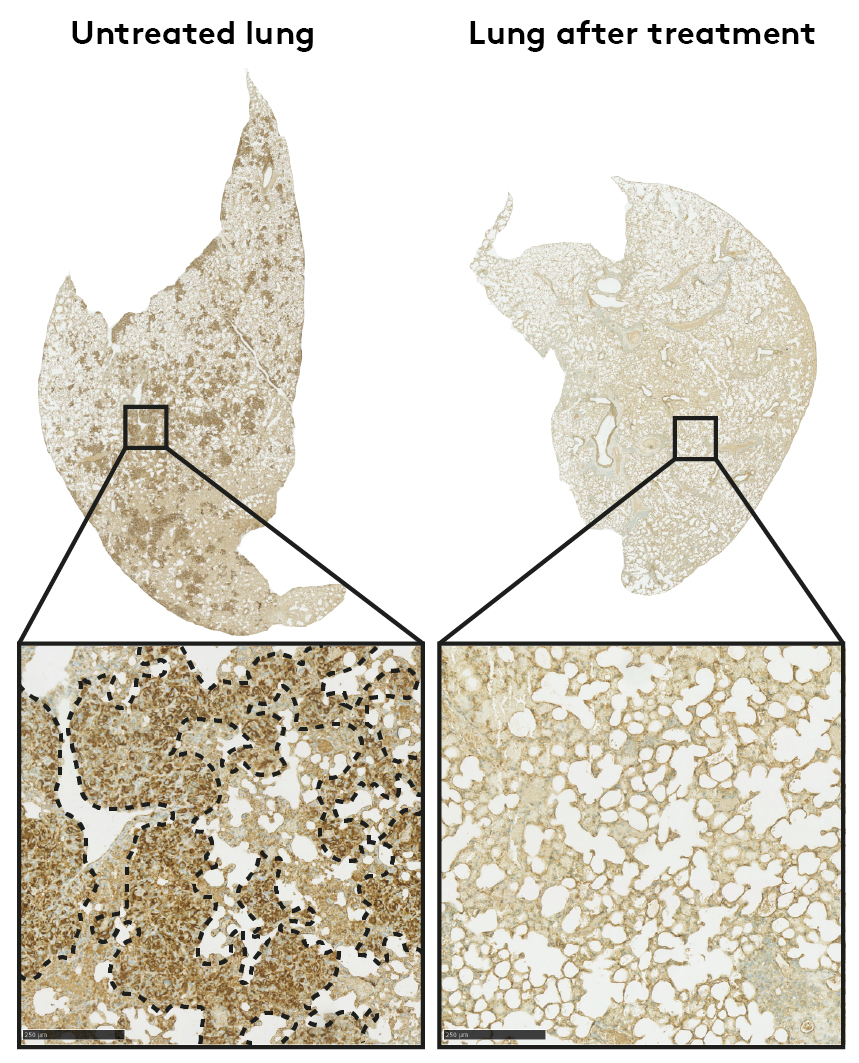
In a new study, researchers from the University of Southern Denmark and Odense University Hospital, in collaboration with CytoVac, have shown that if the lab-cultivated T-cells are administered in combination with drugs that prevent cancer cells from inhibiting the T-cell activity, the effect against the cancer is significantly increased. It can inhibit tumor growth, prevent the spread of cancer, and significantly prolong survival in animal models.
”The spread of cancer is often determining whether a patient can be cured or not. We are particularly impressed by how effective the treatment is in preventing the cancer from spreading.
Positive outcomes, but clinical use will take time
Initially, the treatment has been tested on animals with the breast cancer subtype called triple-negative breast cancer. This type makes up about 10% of all breast cancer cases. It's known for having few effective treatment options and lower survival rates compared to other breast cancers.- In the long term, we aim to offer this combination treatment to patients with triple-negative breast cancer. The only requirement for the patient to receive this treatment would be repeated blood donations. We expect that the the combination treatment also will have effect in other types of cancer, but this remains to be established.
- The first step from here is to test whether we can achieve the same findings in humans who receive the treatment. It is a lengthy process, so it is too early to say when and if patients will benefit from this new combining treatment,' says Odd Gammelgaard.