Non-Alcoholic Fatty Liver Disease (NAFLD) is a highly common condition that affects approximately 24% of the adult population worldwide. The condition itself can be relatively harmless, however, in some patients it progresses to acute inflammatory liver disease (NASH), which can have serious consequences, as this condition can lead to liver cirrhosis and liver cancer.
Early detection is important such that targeted interventions can be initiated to mitigate the progression of the disease. Currently, a liver biopsy is the gold standard to diagnose patients with NASH, but this requires that the patient comes to the hospital to have an invasive procedure performed, with the risk of bleeding. A multitude of blood biomarkers have been assessed for their diagnostic accuracy, but so far none have qualified for clinical use. Consequently, there has until now been an unmet clinical need for non-invasive biomarkers that can diagnose NASH.
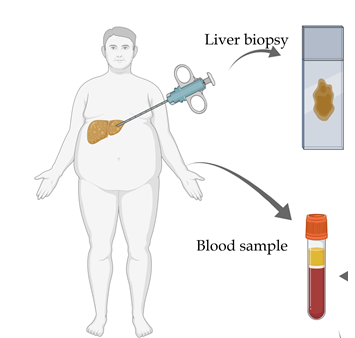
However, this may soon change as researchers in ATLAS and collaborators have discovered TREM2 as non-invasive biomarker for NASH, as the protein can be measured in blood and identify NASH with high diagnostic accuracy.
“It is certainly a new and promising biomarker for NASH that we can detect in a simple blood sample. The new discovery has the potential to contribute to fewer liver biopsies and earlier detection and thereby diagnosis of the patients”, say Vineesh Chandran, postdoc, and Charlotte Wernberg, Ph.D. student, both first authors on the study.
The discovery of TREM2 as a biomarker is an excellent example of translational research, as it began with an observation in a murine NASH model which turned out to be similar in samples from obese patients as well as a validation cohort of over 200 patients with elevated liver stiffness.
Larger validation studies lie ahead with patients recruited from multiple regions to improve the generalizability of NASH diagnosis and to validate proposed rule-in and rule-out cut-off values, and efforts are already in motion to obtain this.
The study was conducted by ATLAS - Center for Functional Genomics and Tissue Plasticity as a collaboration between several research groups from University of Southern Denmark, Odense University Hospital, and Hospital of South West Jutland and others. ATLAS is a center of Excellence funded by the Danish National Research Foundation.
The study is now published in Hepatology