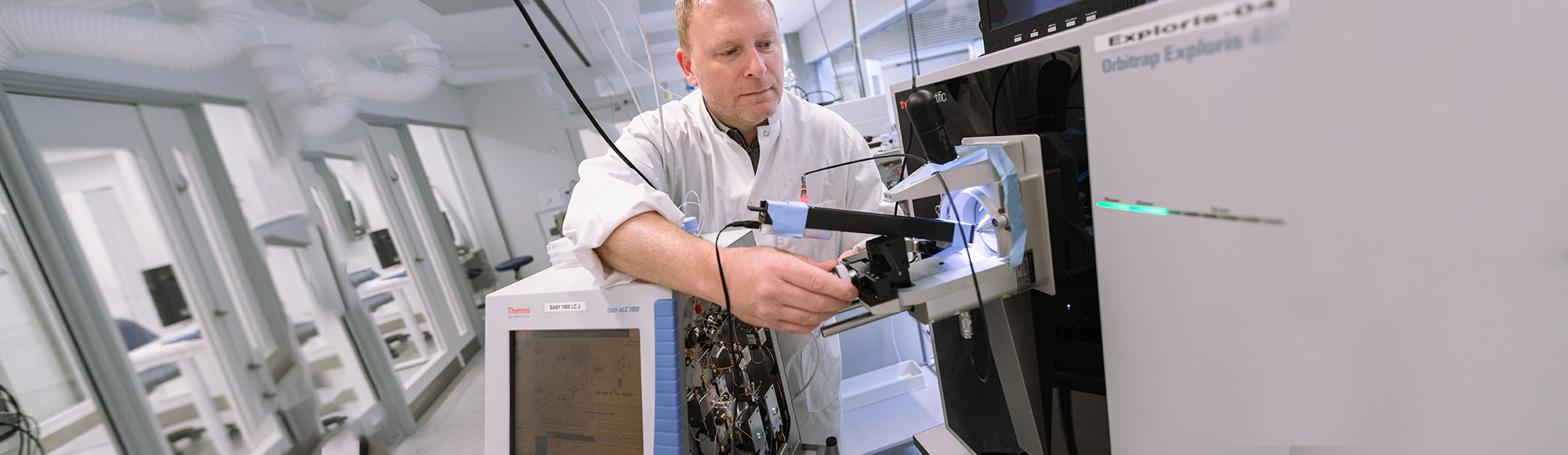
Researcher uses mini-brains for disease research
Professor Martin Røssel Larsen researches brain diseases. In order to better understand them, he makes mini-brains from stem cells in his laboratory.
Neurological diseases such as Alzheimer’s, autism and schizophrenia are complex diseases for which we do not yet have an effective cure, primarily because we do not understand the molecular mechanisms underlying the diseases.
Researchers are trying to understand what happens in a brain affected by these diseases – for example, by studying mice or tissue samples from deceased people who suffered from the disease. However, better methods are necessary before we can hope to cure neurological diseases in the future.
This is the opinion of Professor Martin Røssel Larsen from the Department of Biochemistry and Molecular Biology, who is an expert on studying neural mechanisms at the protein level.
”There are still challenges ahead, and while a mini-brain can never replace a real brain, it does give us far better opportunities to understand neurological diseases and can one day help people suffering from them.
The ethical aspects
– The more insight we can gain into the human brain before and during a neurological disease, the better we are able to understand the disease, which in turn could lead to more effective treatments, he says and continues:
– It goes without saying that we have no desire to extract brain tissue samples from living human beings, but new technology now allows us to work with artificially created cerebral organoids (‘mini-brains’), and this will make a huge difference.
The mini-brains that he cultivates cannot be equated with a brain in a human being. Unlike a human brain, they have no consciousness; they are not a composite entity, and they are nowhere near possessing the same level of complexity. A human brain consists of 86 billion brain cells, whereas a mini-brain consists of approx. 1 million.
Collaboration with British researchers
– This doesn’t mean we shouldn’t discuss the ethical aspects of this field of research, because as techniques improve, mini-brains may become increasingly complex. Still, we’re a long way short of that, says Martin Røssel Larsen.
He and his research team at SDU work closely with Dr Madeline Lancaster, Development Biologist and Head of Research at Cambridge University. In 2013 she, together with the scientific journal Nature, presented one of the world’s first mini-brains at a large-scale press conference.
She has since used mini-brains to study, among other things, the disease microcephaly; a condition in which children are born with abnormally small brains.
Skin cells from sick patients
Madeline Lancaster received skin cells from patients with the disease and made stem cells from them. She then used these stem cells to grow a microcephalic mini-brain and studied it.
During these studies, she was able to identify the developmental defect causing the disease, and this knowledge can now form the basis of therapeutic avenues.
– It’s the same principle that I want to use to study neurological diseases; the only difference being that I will initially be using blood cells rather than skin cells.
Generating a mini-brain from its own cells
Martin Røssel Larsen will also generate mini-brains without neurological diseases, because it is equally important to understand the nature of brain development at a very early stage, which can be equated with the development of a fetal brain.
This will enable us to understand the complex mechanisms that can lead to neurological diseases in the long term.
– I suppose I could always start by making a healthy mini-brain from my own blood cells – a ‘mini-me’, he says jokingly.
Oxygen supply is a challenge
The techniques behind mini-brains are still difficult and far from all universities are working with them. In 2019, Madeline Lancaster estimated that perhaps 100 laboratories worldwide were working on mini-brains.
Currently, there is a physical limit to how large a lab-grown mini-brain can become. Once it reaches a diameter of 5 mm, it stops growing because it does not have the blood supply system of a normal brain to provide the innermost cells with oxygen and nutrients. The inner core of the mini-brain simply dies.
One solution to this problem that Madeline Lancaster has been successful with may be to cut the mini-brain into slices, allowing them to receive nutrients and form more functional nerves and neural networks.
Support from the Independent Research Fund Denmark
– There are still challenges ahead, and while a mini-brain can never replace a real brain, it does give us far better opportunities to understand neurological diseases and can one day help people suffering from them, says Martin Røssel Larsen.
In 2019, Martin Røssel Larsen received research funding from the Independent Research Fund Denmark for a PhD project which aims to develop mini-brains with a view to purifying intact nerve endings and studying the mechanism behind the communication between nerves in the brain.
Photographer: Jacob Fredegaard Hansen
Meet the researcher
Martin Røssel Larsen is a professor at the Department of Biochemistry and Molecular Biology and the research centre Brain Research – Inter Disciplinary Guided Excellence (BRIDGE).